An ageing population
Australians are living longer and dying older. And many will have used aged care services in the eight years before their death.
In 2020, there were 161,300 deaths registered in Australia. Sixty-six per cent of deaths registered in Australia in 2020 were among people aged 75 or over (60% for males and 73% for females). The median age at death was 79 years for males and 85 years for females (AIHW, 2022).
Figure 1: Deaths in Australia by sex and age group, 2020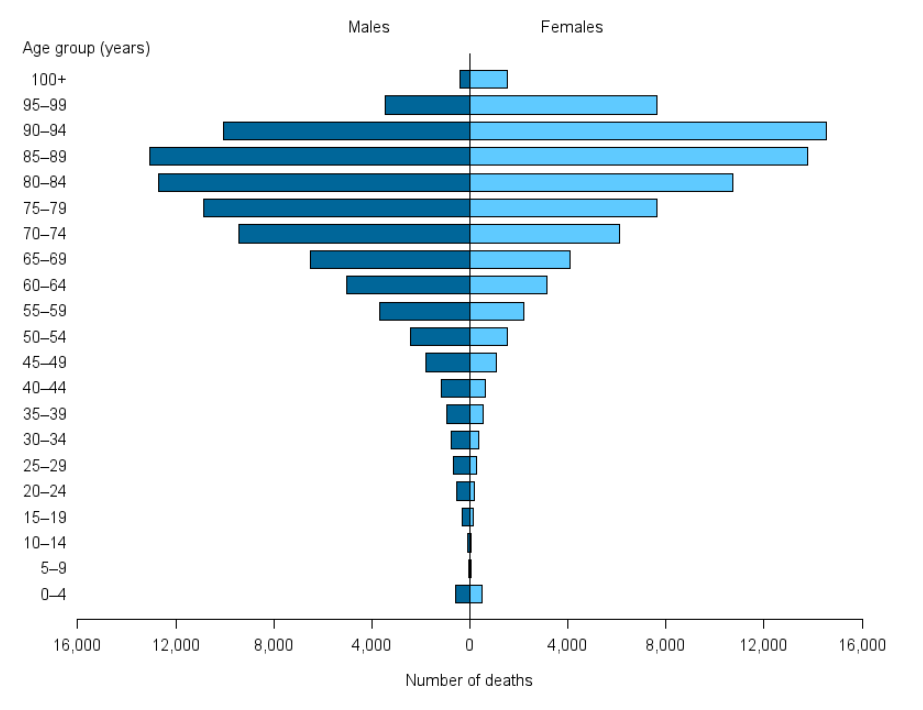 Source: AIHW National Mortality Database (Table S2.1)
Source: AIHW National Mortality Database (Table S2.1)